On the morning of Holden’s surgery, I surprised myself and woke up feeling steady and focused. I had important things to do and there was no time for tears. I managed to keep myself together until the actual moment arrived when I was supposed to hand Holden over to his surgical team so they could take him to the operating room.
“Okay. It’s time,” the nurse said to Sam and me. “We’re ready.”
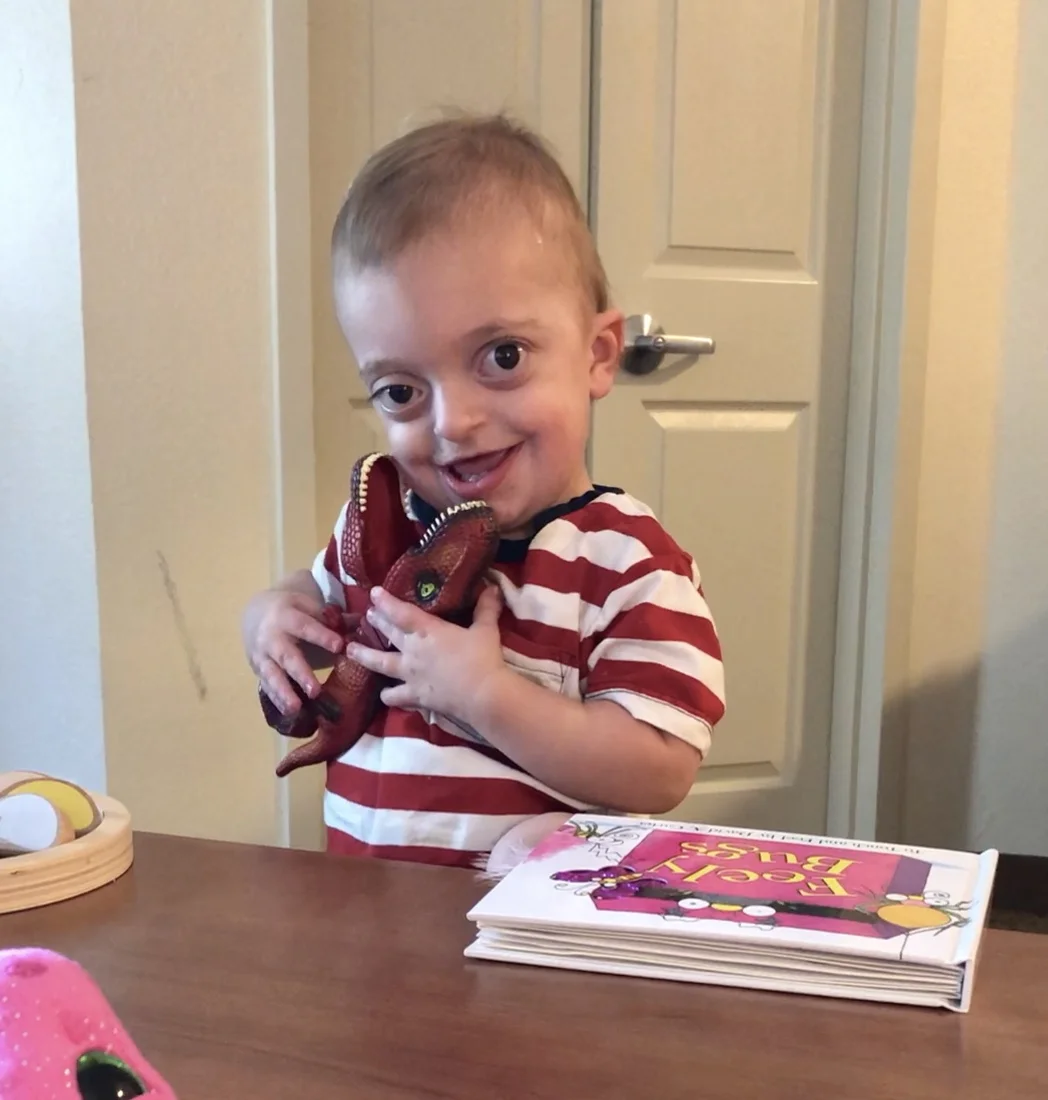
I was not ready. I squeezed my little boy as tight as I could to my chest and walked in the opposite direction.
“Sam,” I whisper-wailed to him. “You have to take Holden from me and give him to them. I can’t do it.”
I was physically incapable of letting my baby go. Sam pried Holden out of my arms and in that moment, I disintegrated. I cried silent tears so thick that I couldn’t even see Holden being taken away from us. However, I sure could hear his pissed off cry!
If you looked at the doctor’s notes about what they were about to do, you would see something like this: lateral canthopexy followed by an anterior cranial vault remodeling with nasal bone graft and lateral tarsorrhaphy.
I am going to attempt to break this down, but parts of it are so complex, I can only hope my understanding is completely accurate.
Lateral canthopexy: This part of his surgery is fairly common and many may recognize this as the medical terminology for a child getting ear tubes. Holden had fluid build up in his ear canals that was causing mild hearing loss. An otolaryngologist surgically placed the tubes in his ears and this should restore his hearing.
Anterior cranial vault remodeling: Once Holden was anesthetized, a craniofacial surgeon cut a smooth, ear-to-ear zig-zag into Holden’s scalp. Then, the skin was peeled back and his skull was exposed. At this point, the craniofacial surgeon took on the role of an architect drafting blueprints for a remodel. He literally, drew his plans with a pencil on Holden’s skull.
Next, a pediatric neurosurgeon came in like a meticulous demolition man and used his tools to physically take apart Holden’s bone. This is called a craniotomy. Once this was completed, the craniofacial surgeon assumed the role of a carpenter and rebuilt Holden’s skull.
Since craniosynostosis syndromes like Holden’s cause premature fusion of the soft spots in the skull, the craniofacial surgeon opened up every space he could within Holden’s head to give his brain room to grow. He also moved Holden’s forehead forward 1.5 cm. Besides providing more room for brain growth, this advancement will help protect Holden’s eyes. The new bone structure that this surgical construction team created inside my son’s head was held in place with dissolvable stitches.
Nasal bone graft: The midface (eyebrows to upper lip) doesn’t grow as fast as the rest of the face in children with Pfeiffer Syndrome. The technical term for this is midface hypoplasia. As a result, a child’s nose usually appears recessed in comparison to the rest of the face. Since the craniofacial surgeon had advanced Holden’s forehead significantly, there was now a substantial gap between his brow and his nose.
As the doctor described it: “I sliced a piece of bone off of his brow like you would slice a piece of beef carpaccio.” He then took that fragment of bone and connected it from Holden’s forehead to his nose, forming a bridge between the two that was held in place with dissolvable stitches.
Lateral tarsorrhaphy: This means that the craniofacial surgeon sewed Holden’s eyes shut to protect them from damage both during and after his surgery. The pressure and swelling a child experiences after an anterior cranial vault remodeling is extreme and there is a risk of eye damage and vision loss. Post-operatively, the only stitches that were left in Holden’s eyes are in the far corners, so he can still see while he is healing. The stitches are dissolvable and should be gone in about a month.
While all of this was happening to our son, Sam and I stayed busy, trying not to think about the procedures our son was undergoing a few walls away. Sam did some work. I watched Netflix. We were given a direct extension to dial in to the operating room and check in on how Holden was doing. After about 5 hours, I dialed the extension for the last time.
“He’s up and he’s mad,” the nurse told me. “He wants his mama.”
I looked over at Sam who was staring at me, standing completely still, waiting to hear the latest news.
“He’s up. He made it,” I said, exhaling for the first time all morning. In that moment we shed happy tears. Our boy was going to be okay.